Dental Implants Procedure & Recovery
Medically Reviewed by: Dean Vafiadis, DDS
On this page: Implant consultation | Procedure details | Recovery & Aftercare | Implant types
Dental implants are artificial tooth roots used to support a restoration for a missing tooth or teeth, helping to stop or prevent jaw bone loss. The implantation procedure is categorized as a form of prosthetic (artificial replacement) dentistry, but also is considered a form of cosmetic dentistry.
People who have lost teeth might feel too self-conscious to smile or talk. Additionally, biting irregularities caused by tooth loss can have a negative effect on eating habits, leading to secondary health problems like malnutrition.
By replacing missing tooth roots, dental implants provide people with the strength and stability required to eat all the foods they love, without struggling to chew. Additionally, they help to stimulate and maintain jaw bone, preventing bone loss and helping to support facial features.
Tooth Loss

- Tooth decay
- Root canal failure
- Gum disease (Periodontitis)
- Trauma to the mouth (tooth injury)
- Excessive wear and tear
- Congenital defects
Consultation
To determine if implants are right for you, a consultation with your dentist, oral surgeon, and/or periodontist or prosthodontist is needed. During this appointment, your dental professional will thoroughly examine your teeth and gums and evaluate bone density and quantity. This may involve X-rays and computer tomography scans (CT scans) to ensure there is sufficient bone structure for placing the implant(s), and to determine exactly where they should be placed.
Based on the condition of your oral tissues, oral hygiene and personal habits, and commitment to follow aftercare instructions, your dentist will advise you of the most appropriate treatment plan. Some patients with insufficient bone or gum tissue require bone or soft tissue grafts and/or the use of small diameter implants (also called mini implants).
Depending on your situation, your dental professional will advise you of how long the entire treatment process will take, how many appointments will be necessary and what you can expect after each procedure. During the consultation, options for local anesthesia (to numb the affected and surrounding areas) and sedation dentistry, if necessary, also will be discussed. The estimated cost of your dental implants will also be discussed during this meeting. Costs can vary significantly based on the type of treatment you opt for (amongst other things).
Before Treatment
Any underlying oral health issues must first be managed before implantation may be considered. Common issues such as tooth decay and gum disease can make treatment less effective.
If you are a smoker, your dentist will advise you to quit, as smokers face a greater risk of failure than non-smokers. Smoking can affect osseointegration, the process by which a dental implant anchors to the jaw bone.
Once your dentist deems your mouth healthy enough for treatment, your custom treatment can begin.
Placing Your Implant(s) – The Procedure
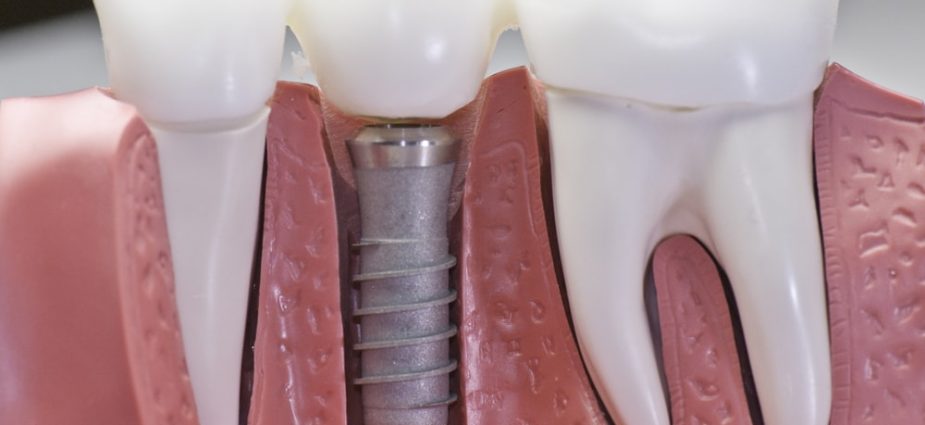
Today’s dental implant restorations are virtually indistinguishable from other teeth. This appearance is aided in part by the structural and functional connection between the implant and the living bone. The procedure is typically performed in a single sitting but requires a period of osseointegration.
Osseointegration is the process by which the implant anchors to the jaw bone. An osseointegrated implant takes anywhere from six weeks to six months to anchor and heal, at which point your dentist can complete the procedure by placing a crown, bridge or hybrid denture restoration. If osseointegration does not occur, the implant will fail.
Dental implantation, which is performed to replace missing teeth, can be done any time after adolescence or when bone growth is complete. Certain medical conditions, such as active diabetes, cancer or periodontal disease, may require additional treatment before the procedure can be performed.
Detailed procedural steps are as follows:
Preparing the Jaw for Implantation: A dental implant and its restoration is commonly composed of a titanium material screw and a crown. A small-diameter hole (pilot hole) is drilled at edentulous (where there is no tooth) jaw sites in order to guide the titanium implant fixture in place. To avoid damaging vital jaw and face structures like the inferior alveolar nerve in the mandible (lower jaw), a dentist must use great skill and expertise when boring the pilot hole and sizing the jaw bone. In many instances dentists use surgical guides created based on the CT scans when placing the implants.
Placement: After the initial pilot hole has been drilled into the appropriate jaw site, it is slowly widened to allow placement of the implant screw. Once in place, surrounding gum tissue is secured over the implant and a protective cover screw is placed on top to allow the site to heal and osseointegration to occur. After up to six months of healing, your dentist will uncover the implant and attach an abutment (which holds the crown or tooth-like replacement). In some cases, the abutment may be attached during the initial procedure. When the abutment is in place, your dentist then will fabricate a temporary or final crown. Sometimes the final crown can be fabricated on the same day that the abutment is placed. The temporary crown serves as a template around which the gum grows and shapes itself in a natural way if warranted. The process is completed when the temporary crown is replaced with a final crown.
Recovery, Follow-up & Aftercare
Dental implant recovery depends on a number of factors, one of which includes the various procedures required to complete your treatment. However, it is generally recognized that once an implant has been placed, maintaining diligent oral hygiene habits helps ensure proper integration with bone structure. Failure to floss and brush can contribute to failure of the treatment. Infection can occur if the implant and surrounding areas are not cleaned properly. Smoking also is attributed to high failure rates and should be avoided following implant procedures.
If provisional restorations were placed along with the implant(s), it will be important to clean them as you would your natural teeth to ensure the best possible healing and fusing.
After the initial surgical procedure, discomfort should be minimal. Swelling of your gums and face may occur, as well as minor bleeding and bruising of the implant site. Prescription pain medications may be prescribed by your dentist to relieve any pain or discomfort you feel after the procedure. For five to seven days after surgery, your diet should be restricted to soft foods. If stitches are present, they may need to be removed by your dentist; however, self-dissolving stitches that do not require removal are typically used.
Healing from the surgical procedure to place the implant(s) takes up to six months, while the fitting and seating of the crown(s) can take up to two months. Again, this timeframe depends on individual cases and treatments. Follow-up appointments with your treatment coordinators are essential for monitoring your progress.
If cared for properly, it can remain in place for a lifetime.
Types of Dental Implants
More than 60 companies manufacturer dental implants and/or the materials used to create the restorations placed on top of them. As a result, dentists have many options for identifying the right treatment for specific patient needs. However, be aware that if you undergo an implant procedure by one dentist, then see a different dentist for a repair, your new dentist may have limited experience with, or may not have access to, the material components used by the previous dentist.
Dental implants usually are categorized based on the type of procedure used to place them: two-stage or single stage.
Two-Stage Implants: A two-stage procedure involves surgery to place the implant into the jaw bone and close (stitch) the gum tissue. Several months after healing, a minor surgery is performed to attach an abutment and temporary restoration.
Endosteal (Endosseous) Implants: Placed in the jaw bone, endosteals are the most commonly used type for two-stage implant procedures. Placed primarily as an alternative to a bridge or removable denture, endosteal implants include screw types (threaded), cylinder types (smooth) or bladed types.
Single-Stage Dental Implants: A single-stage procedure involves surgically placing a longer implant into the jaw so it is on the jaw bone, with the top level with the gum tissue, after which the gum tissue is closed (stitched), leaving the implant healing cap visible. As a result, after several months of healing, the abutment and temporary restoration can be attached without the need for minor surgery to expose the head.
Subperiosteal Implants: Placed on the jaw bone within the gum tissue, with the metal implant post exposed to hold the restoration, subperiosteals are rarely if ever used today. Subperiosteals were primarily used to hold dentures in place in patients with insufficient bone height.
Coatings
Although most dental implants are made of titanium, the surface — which affects the long-term integration and stability of treatment — can vary. A porous surface contributes to more bone contact than a machined titanium surface. Other surfaces include a grit-blasted or acid-etched and roughened surface, a microgrooved or plasma-sprayed titanium surface, and a plasma-sprayed hydroxyapatite coating, and Zirconia (nonmetal).
Connectors
Implants also may be categorized based on the shape/type of their head. All implants require the restoration and abutment to be attached or screwed to the head. For this purpose, there are three main connector types:
Internal Hex Connectors: Shaped like a hexagon, an internal hex connector is an opening in the implant head into which the restoration/abutment is screwed.
External Hex Connectors: Also shaped like a hexagon, these connectors are atop the implant head.
Internal Octagon Connectors: Shaped like an octagon, an internal octagon connector has an opening in the implant head into which the restoration/abutment is screwed.
Implant Sizes
Another way to categorize implants is based on their size (also called platform), which dictates where they generally can be placed in the mouth. However, every case is different, and individual spacing and bone availability needs may dictate the use of a different size. The fixture has a platform dimension as well as length, both being important criteria in fixture selection.
Standard Platform: Standard dental implants range in size from 3.5 mm to 4.2 mm in diameter. These comparatively shorter and narrower implants are most commonly placed toward the front of the mouth.
Wide Platform: Wide platform dental implants range in size from 4.5 mm to 6 mm in diameter and are placed primarily in the back of the mouth.
Mini or Narrow Body: Mini or narrow body dental implants range in size from 2 mm to 3.5 mm in diameter and are placed primarily in patients with insufficient space between their tooth roots to accommodate a larger size. They also may be placed when the patient has insufficient bone density. They are sometimes utilized as temporary support for provisional prostheses while the final conventional dental implants are osseointegrating.
[updated Feb 5, 2019]
About the Reviewer
 Dr. Dean Vafiadis is the founder of New York Smile Institute, a premier Manhattan dental studio devoted to restoring and enhancing the natural beauty of the smile using conservative, state-of-the-art practices. Dr. Dean is an Associate Professor of Prosthodontics at NYU College of Dentistry and serves as the Director of the Full-Mouth Rehabilitation CE course at NYU. He lectures nationally and internationally on various topics such as Aesthetics, implant designs, computer restorations, ceramic materials, occlusion and more. Learn More
Dr. Dean Vafiadis is the founder of New York Smile Institute, a premier Manhattan dental studio devoted to restoring and enhancing the natural beauty of the smile using conservative, state-of-the-art practices. Dr. Dean is an Associate Professor of Prosthodontics at NYU College of Dentistry and serves as the Director of the Full-Mouth Rehabilitation CE course at NYU. He lectures nationally and internationally on various topics such as Aesthetics, implant designs, computer restorations, ceramic materials, occlusion and more. Learn More






